Right Ventricular Failure
PEARLS
- Find and treat the cause (e.g. PE, ARDS, MV failure, fluid overload, pulmonary HTN)
- Management focuses on: volume and preload optimisation / RV contractility / RV afterload reduction
OVERVIEW
- Mortality as high as LV failure
- Patients with HFrEF / HFpEF with Left Heart Failure (LHF) have worse prognosis if they have concomitant RHF
- Normal RV function is governed by SVR (systemic venous return), Pulmonary Vascular Resistance (PVR) (RV afterload), pericardial compliances, native contractility of the RV free wall and interventricular septum
- Afterload is the primary determinant of normal RV function and RVEF is inversely proportional to PAP
- RV is better suited to changes in volume than pressure due to compliance and the thin free wall but when the RV afterload increases for whatever reason –> the RV dilates
- As RV dilates –> promotes TR –> worsens RV dilation –> vicious cycle of ‘auto-aggravation’ (shift to descending portion of the Frank-Starling curve)
- With severe RV dilation –> mechanical flattening of the interventricular septum (left shift) with increased LVEDP (LV end-diastolic pressure) –> reduced LV preload
- Termed: Ventricular interdependent filling
- Elevated right heart pressures –> coronary sinus congestion –> reduction of coronary blood flow –> can provoke RV ischaemia
- Venous congestion also affects: liver / renal function / fluid retention –> Which may also worsen RHF
CAUSES
Primary
- volume/pressure overload: LVF, PE, ARDS, amniotic fluid embolism
- mechanical: MV
- sepsis
- cardiac: cardiomyopathies, ARVD, TV rupture, tricuspid or pulmonary regurgitation
Secondary
- respiratory: cor pulmonale, OSA, COPD
- muscular disease
- neuromuscular; poliomyelitis, amyotrophic lateral sclerosis, muscular dystrophy
- connective tissue: SLE, CREST, RA, hepatic porto-pulmonary syndrome
- cardiac: LVF, intra-cardiac shunt, cardiomyopathies
CLINICAL FEATURES
- raised JVP with a prominent V wave from TR
- low cardiac output and hypotension –> cardiogenic shock
- hepatic enlargement (depending on chronicity), ascites
- peripheral oedema (may or may not have this)
- Other features:
- Precordial heave
- If secondary to pulmonary hypertension –> loud P2
- An increase in the amplitude of the systolic murmur during inspiration (Carvallo sign) may distinguish TR from MR
INVESTIGATIONS
- Bloods: NT-proBNP (may be difficult to interpret as is not specific to right heart), elevated troponins (useful in prognostication), LFTs (cholestatic picture in chronic failure with synthetic function impairment, transaminitis in acute), EUCs
- CXR:
- Cardiac silhouette may appear globular
- Loss of retrosternal airspace on lateral –> RV enlargement
- Rightward displacement of the cardiac silhouette well beyond the spin –> RA enlargement
- If PH: main PA enlarged
- May see cause of PH — i.e. COPD
- ECG: Right axis deviation, sinus tachycardia, atrial arrhythmias (common), SI/QIII/TIII (high specificity / low sensitivity), RV Strain pattern. E.g: PE ECGs, RVH ECGs
- TTE / TOE:
- RV dilation (can grossly compare w/ LV size on AP4C)
- Diastolic interventricular septal flattening (left-ward shift) = volume overloaded state
- Systolic interventricular flattening (left-ward shift) = pressure overloaded state
- RV hypokinesis (mild, moderate, severe)
- Look at TAPSE and RVFAC (TAPSE <17mm, RFAC <35% are abnormal)
- Right heart catheterisation: elevated pressures
- cMRI: Gold standard of quantitative non-invasive measurement of RV volume, mass and EF
MANAGEMENT
Focuses on:
- Fixing the underlying cause (if you’re able to)
- Management of volume and preload
- RV contractility
- RV afterload
Management of volume and preload
- Aim for CVP 8-12mmHg
- May require judicious fluid boluses –> If not volume responsive stop
- if volume overloaded reduce preload;
- Fluid and salt restriction
- Aggressive diuretic therapy (mainstay: loop diuretics. Consider addition of thiazides, and aldosterone antagonist)
- Renal Replacement Therapy (RRT) should be reserved for those who are refractory to diuresis (UNILOAD and CARRESS-HF Trials)
- sequential TTE/TOE, PAC, or right heart catheterisation may be helpful in fluid titration
RV Contractility with Inotropes and Vasopressors
- If CO / BP inadequate –> Commence inotropes
- no selective right heart inotrope exists
- Inotropes:
- beta-agonists, calcium sensitisers and phosphodiesterase inhibitors (PDEIs)
- must decrease afterload or else increased contractility with increased myocardial O2 consumption will take place
- levosimendan: shown to reduce PVR and improve RV function
- milrinone: increased contractility via a non-beta-adrenergic mechanisim –> does not increase myocardial oxygen demand
- To maintain perfusion use vasopressors:
- Adrenaline, noradrenaline, phenylephrine and vasopressin: increase MAP and thus coronary perfusion but if not appropriately used will increase myocardial O2 consumption by increasing afterload too much
- Vasopressin may be preferentially used given it has less effect on PVR as well as its renal effect via selective efferent arteriole constriction
- Digoxin: Unknown if beneficial, although may improve CO
Afterload Reduction
- Minimise PVR: avoid hypoxia, acidaemia, alveolar distension
- Consider GTN / SNiP –> may be at the cost of reduced coronary perfusion
- Consider role of: RAASi, B-blockers, hydralazine
- Selective pulmonary vasodilators:
- prostaglandins (INH, IV, SC): increased NO release
- NO: pulmonary vasodilator, oxygenation and PVR improve but no mortality benefit, rebound pulmonary hypertension observed
- sildenafil and tadalafil (PDE-III inhibitor): oral medication, phosphodiesterase enzyme
- milrinone (Mostly a PDE-III inhibitor, does also have some PDE-V inhibition): decreases PVR, can be given IV or nebulised
- Endothelin receptor antagonists: Early trials are promising –> Bosentan
- recombinant BNP: neseritide, reduces preload and afterload -> improved Q without inotropy (increased mortality + renal failure)
Mechanical Ventilation and PEEP
- distending alveolar pressure transmitted through pulmonary capillary bed –> determines the opening pressure of pulmonary valve
- PEEP contributes to augmentation of preload because of transmitted pressure to RV
- low TV
- Avoid gas trapping (watch PEEP!)
Surgical Intervention and RV Support
- Valvular surgery:
- TV surgery (for TR or TS)
- Would be unusual for PV lesion, however should be considered
- MV repair / replacement
- Biventricular pacing for resynchronisation
- Mechanical Cardiac Support
- RVAD (LVAD if LVF is the cause of RVF)
- VA-ECMO
- Transplant
- Palliative procedure such as balloon atria septostomy (BAS)
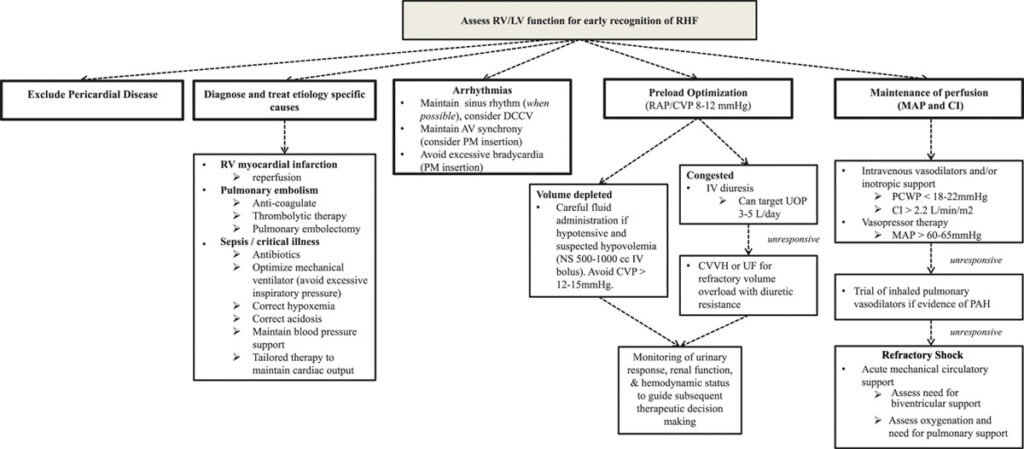
Figure 11. Management of acute right-sided heart failure. All management must be undertaken with an awareness of the patient’s hemodynamic status. If this status is not clear clinically, then invasive assessment/monitoring should be undertaken. Hemodynamic targets provide rough guidelines for tailored therapy. AV indicates atrial-ventricular; CI, cardiac index; CVP, central venous pressure; CVVHF, continuous venovenous hemofiltration; DCCV, direct current cardioversion; IV, intravenous; LV, left ventricular; MAP, mean arterial pressure; NS, normal saline; PAH, pulmonary arterial hypertension; PCWP, pulmonary capillary wedge pressure; PM, pacemaker; RAP, right atrial pressure; RHC, right-sided heart catheterization; RV, right ventricular; UF, ultrafiltration; and UOP, urine output.
SUMMARY OF TREATMENT OPTIONS
- Treat the cause!
- Simple things:
- Oxygenation
- Mechanical ventilation — aggressively treat hypercarbia, acidosis (all increase PVR)
- Management of volume and preload
- Target CVP 8-12 if able
- RV contractility
- vasodilators + inotropes
- milrinone (50mcg/kg bolus -> 0.2-0.8mcg/kg/min) [caution with bolus administration]
- RV afterload
- sildenafil 50-100mg PO preoperatively
- inhaled nitric oxide 20-40ppm (good in bypass, doesn’t cause systemic hypotension as inactivated when bound to Hb)
- inhaled prostacyclin (increases cAMP) – 50mcg in saline nebulised every hour OR 50ng/kg/min nebulised into inspiratory limb
- IV prostacyclin (if inhaled not available) – 4-10ng/kg/min
- pacing to improve A-V synchrony / biventricular device
- Surgery
- RVADs
- Transplant
References and Links
- Wiesbauer F. Medical Treatment of Heart Failure. Medmastery
- Lahm T, McCaslin CA, Wozniak TC, Ghumman W, Fadl YY, Obeidat OS, Schwab K, Meldrum DR. Medical and surgical treatment of acute right ventricular failure. J Am Coll Cardiol. 2010 Oct 26;56(18):1435-46. doi: 10.1016/j.jacc.2010.05.046. Review. PubMed PMID: 20951319. [Free Full Text]
- Walker LA, Buttrick PM. The right ventricle: biologic insights and response to disease: updated. Curr Cardiol Rev. 2013 Feb 1;9(1):73-81. Review. PubMed PMID: 23092273; PubMed Central PMCID: PMC3584309.
- Konstam MA, Kiernan MS, Bernstein D, Bozkurt B, Jacob M, Kapur NK, Kociol RD, Lewis EF, Mehra MR, Pagani FD, Raval AN, Ward C; American Heart Association Council on Clinical Cardiology; Council on Cardiovascular Disease in the Young; and Council on Cardiovascular Surgery and Anesthesia. Evaluation and Management of Right-Sided Heart Failure: A Scientific Statement From the American Heart Association. Circulation. 2018 May 15;137(20):e578-e622. doi: 10.1161/CIR.0000000000000560. Epub 2018 Apr 12. PMID: 29650544. [Free Full Text]
- Costanzo MR, Guglin ME, Saltzberg MT, Jessup ML, Bart BA, Teerlink JR, Jaski BE, Fang JC, Feller ED, Haas GJ, Anderson AS, Schollmeyer MP, Sobotka PA; UNLOAD Trial Investigators. Ultrafiltration versus intravenous diuretics for patients hospitalized for acute decompensated heart failure. J Am Coll Cardiol. 2007 Feb 13;49(6):675-83. doi: 10.1016/j.jacc.2006.07.073. Epub 2007 Jan 26. Erratum in: J Am Coll Cardiol. 2007 Mar 13;49(10):1136. PMID: 17291932.
- Bart BA, Goldsmith SR, Lee KL, Givertz MM, O’Connor CM, Bull DA, Redfield MM, Deswal A, Rouleau JL, LeWinter MM, Ofili EO, Stevenson LW, Semigran MJ, Felker GM, Chen HH, Hernandez AF, Anstrom KJ, McNulty SE, Velazquez EJ, Ibarra JC, Mascette AM, Braunwald E; Heart Failure Clinical Research Network. Ultrafiltration in decompensated heart failure with cardiorenal syndrome. N Engl J Med. 2012 Dec 13;367(24):2296-304. doi: 10.1056/NEJMoa1210357. Epub 2012 Nov 6. PMID: 23131078; PMCID: PMC3690472.
[cite]

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at the Alfred ICU in Melbourne. He is also a Clinical Adjunct Associate Professor at Monash University. He is a co-founder of the Australia and New Zealand Clinician Educator Network (ANZCEN) and is the Lead for the ANZCEN Clinician Educator Incubator programme. He is on the Board of Directors for the Intensive Care Foundation and is a First Part Examiner for the College of Intensive Care Medicine. He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives.
After finishing his medical degree at the University of Auckland, he continued post-graduate training in New Zealand as well as Australia’s Northern Territory, Perth and Melbourne. He has completed fellowship training in both intensive care medicine and emergency medicine, as well as post-graduate training in biochemistry, clinical toxicology, clinical epidemiology, and health professional education.
He is actively involved in in using translational simulation to improve patient care and the design of processes and systems at Alfred Health. He coordinates the Alfred ICU’s education and simulation programmes and runs the unit’s education website, INTENSIVE. He created the ‘Critically Ill Airway’ course and teaches on numerous courses around the world. He is one of the founders of the FOAM movement (Free Open-Access Medical education) and is co-creator of litfl.com, the RAGE podcast, the Resuscitology course, and the SMACC conference.
His one great achievement is being the father of three amazing children.
On Twitter, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
ICU Advanced Trainee BMedSci [UoN], BMed [UoN], MMed(CritCare) [USyd] from a broadacre farm who found himself in a quaternary metropolitan ICU. Always trying to make medical education more interesting and appropriately targeted; pre-hospital and retrieval curious; passionate about equitable access to healthcare; looking forward to a future life in regional Australia. Student of LITFL.

